 May, 22 2024
May, 22 2024
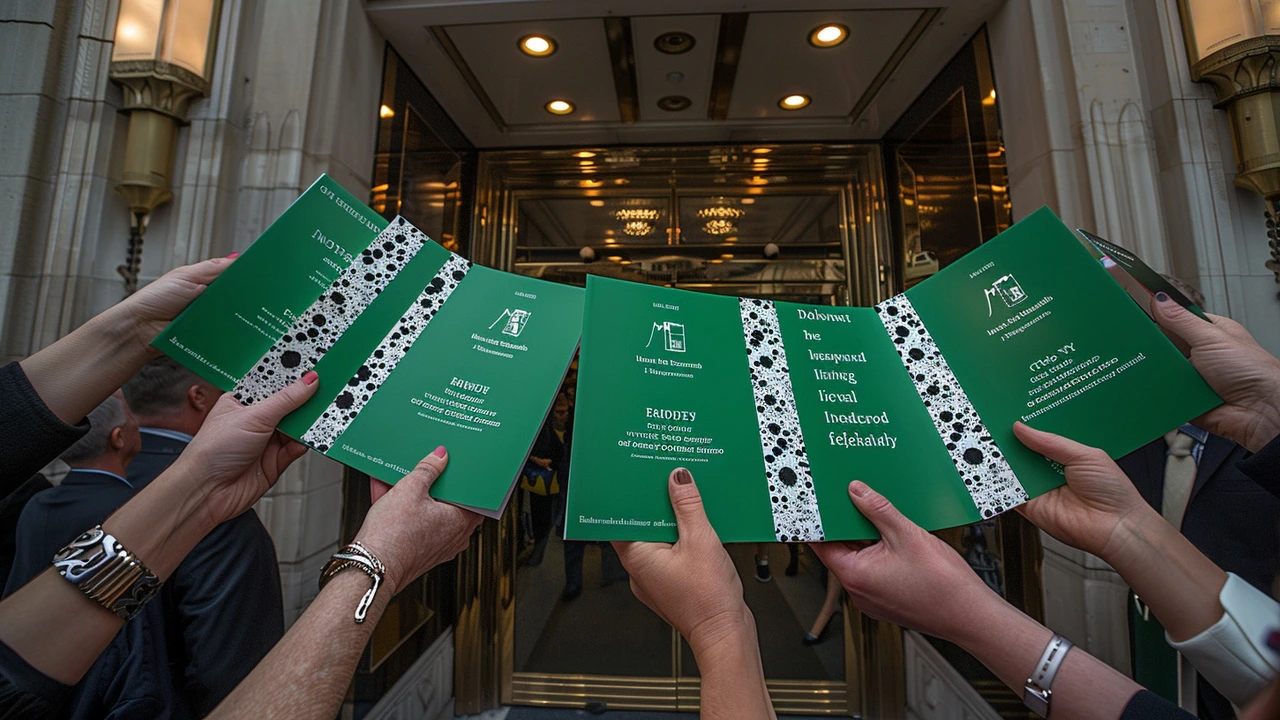
The Infected Blood Inquiry: Unmasking a Health Scandal
The release of the final report from the Infected Blood Inquiry marks a watershed moment in one of the deepest health scandals to have plagued the UK. The inquiry, which meticulously scrutinized decades of evidence, delivered a sobering account of the systematic failures that led to thousands of people receiving contaminated blood, resulting in numerous deaths and chronic health issues for victims and their families. It painted a grim picture of a health system that, at best, was complacent and, at worst, grossly negligent in its duty to protect patients.
At the heart of the inquiry's findings is the revelation that people were consistently misled about the safety of the treatments they were receiving. Patients and their families were not given an accurate picture of the risks, and in many instances, information that could have prevented harm was withheld. The report emphasizes that state institutions failed to come clean about their mistakes, choosing instead to avoid admitting any wrongdoing and delaying compensation. This evasion of responsibility not only compounded the suffering of victims but also eroded public trust in health services.
Recommendations: A Path to Justice
To address these historical failings, the inquiry has put forward a series of recommendations aimed at rectifying past wrongs and preventing future occurrences. Paramount among these is the call for immediate compensation for victims and their families. The report suggests that a fair and quick resolution through financial redress is essential not only for the victims' material well-being but also as a step towards acknowledging their suffering.
Another key recommendation is the establishment of a statutory duty of candour for civil servants. This measure is intended to ensure that those in positions of authority are legally obligated to be transparent and truthful, particularly when lives may be at stake. Additionally, the report calls for a comprehensive overhaul of clinical training to include robust protocols for preventing and managing such critical failures. These recommendations are designed to rebuild trust and ensure that healthcare providers are better equipped to serve the public without repeating the mistakes of the past.
The Three Crucial Questions
The success of the Infected Blood Inquiry now hinges on addressing three pivotal questions. The first question is whether the government will implement these recommendations, especially the compensation proposals, without delay. Swift and decisive action on this front is critical for conveying a sincere commitment to justice. The second question concerns accountability - who will ensure that the government follows through on these recommendations? The Public Administration and Constitutional Affairs Committee could play a significant role by providing oversight and holding the government to its promises.
The third, and perhaps the most challenging question, is whether the state can act to prevent similar tragedies in the future. Learning from the past is vital. The report highlights other instances of systematic failures, such as the miscarriage of justice involving postmasters and the scandals in maternity services, suggesting a pattern of neglect that needs to be addressed. This calls for a cultural shift within public services, prioritizing transparency, accountability, and the unwavering protection of citizens' welfare.
Implementation Challenges and Accountability
Implementing the recommendations will require more than just political will; it will also necessitate a coordinated effort across various arms of the government and health sectors. Financial logistics for compensation, legislative changes for the duty of candour, and curriculum adjustments in medical education must all be synchronized to ensure a holistic response to the inquiry's findings. The government's ability to mobilize these resources and effect change will be a litmus test of its commitment to righting historical wrongs.
Accountability mechanisms are equally crucial. The establishment of independent oversight bodies, potentially modeled after the Public Administration and Constitutional Affairs Committee, could provide the necessary checks and balances. Such bodies must be empowered to review government actions critically and hold policymakers responsible for their decisions. This accountability, embedded within a transparent and robust framework, will go a long way in preventing the recurrence of similar health scandals.
Ensuring Future Safety in Healthcare
Looking to the future, the state must embrace a proactive stance in safeguarding health services against systemic failures. Policies must prioritize patient safety, with real-time monitoring and swift interventions where anomalies are detected. Continuous training and education for healthcare professionals, focusing on ethical practices and patient-centered approaches, are essential. The integration of advanced technologies for tracking and managing health records could also add an extra layer of security against potential risks.
The broader public must also be involved in this journey. Public awareness campaigns about patient rights, the intricacies of health policies, and avenues for redress can empower individuals to advocate for better services. Building a culture of vigilance within the community will act as a supplemental force driving accountability from the grassroots level up to policymakers.
Reflecting on the Road Ahead
The Infected Blood Inquiry has shed light on a dark chapter in the UK's healthcare history, but it has also provided a roadmap for a future built on accountability and justice. Implementing its recommendations is just the beginning. The real challenge lies in maintaining the momentum for change and ensuring that the lessons learned translate into tangible improvements in healthcare delivery and policy formulation.
Ultimately, it is a test of the government's resolve and the collective will of society to rectify past mistakes and prevent future tragedies. The victims and their families deserve nothing less than an unwavering commitment to justice, transparency, and reform. It is a commitment that will define the legacy of the Infected Blood Inquiry and the resilience of the public health system.

love monster
May 22, 2024 AT 18:57The longitudinal data sets reveal a cascade of risk assessment failures that were compounded by opaque governance frameworks. From a systems engineering perspective, the lack of a feedback loop in the hemophilia treatment protocols created an environment ripe for contamination. Moreover, the inter‑agency communication breakdown violated standard operating procedures for high‑risk biologics. This aligns with the concept of latent conditions in safety science, where hidden variables aggregate to produce catastrophic outcomes. The inquiry’s emphasis on a statutory duty of candour could serve as a corrective control mechanism, provided it is paired with robust audit trails. In practice, implementing real‑time surveillance dashboards would mitigate future exposure. Finally, aligning compensation protocols with actuarial models ensures equitable redress for affected families while preserving fiscal sustainability.
Christian Barthelt
May 22, 2024 AT 19:47The report’s phrasing frequently oscillates between "systemic failure" and "isolated error," which is a glaring inconsistency. One must question why the authors do not adhere to a single terminology throughout; precision matters, especially in policy documents. While the recommendations are well‑intentioned, without a clear implementation roadmap, they risk becoming another white‑paper exercise. The omission of a statutory timeline for compensation is particularly troubling. In short, noble ideas need concrete scaffolding to avoid becoming mere rhetoric.
Ify Okocha
May 22, 2024 AT 20:37The narrative conveniently glosses over the human cost, reducing tragedy to a series of bureaucratic blunders. Victims were forced to navigate a labyrinth of red tape while their health deteriorated, a reality that the report barely acknowledges. The failure to disclose risk information constitutes a breach of informed consent, a principle that should be sacrosanct in any modern healthcare system. By sidestepping accountability, the state perpetuates a culture of impunity. The inquiry’s recommendations, though comprehensive on paper, lack the teeth to enforce real change. This is not just a policy oversight; it is a moral failure that demands urgent redress.
William Anderson
May 22, 2024 AT 21:27One could argue that the inquiry is a masterclass in bureaucratic largesse, yet the actual substance feels dreadfully thin. The authors wax lyrical about “statutory duties” while offering no specifics on enforcement mechanisms. It’s a classic case of grandiloquent language masking a paucity of actionable steps. The narrative drifts into pseudo‑scholarly meanderings, leaving the reader yearning for a concrete plan. In short, the report reads like an elaborate apology that forgets to mention the apology itself.
Sherri Gassaway
May 22, 2024 AT 22:17In contemplating the ethical dimensions of this scandal, one is reminded of the ancient maxim that knowledge without compassion is hollow. The duty of candour, as posited, must transcend legal obligations and become a lived ethic within the health bureaucracy. If we merely codify transparency without fostering an institutional culture that values truth‑telling, the reforms will collapse under their own weight. Thus, the inquiry should have devoted more space to the philosophical underpinnings of trust and the moral calculus that guides public service.
Milo Cado
May 22, 2024 AT 23:07It’s encouraging to see the inquiry finally acknowledging the depth of the injustices. 💪 The recommendation for swift compensation aligns with the principle of restorative justice, and I hope the government treats it with the urgency it deserves. A statutory duty of candour could rebuild public trust if implemented transparently. Let’s keep the conversation focused on actionable steps and support the victims every step of the way. 🙏
MONA RAMIDI
May 22, 2024 AT 23:57Honestly, the whole saga feels like a tragic opera where the chorus of victims never gets a solo. The recommendations are a decent script, but without a decisive director, we’ll just watch the same drama unfold. It’s time for the state to step off the sidelines and actually fund the compensation it promises. Anything less is a cruel encore for those already suffering.
grace riehman
May 23, 2024 AT 00:47The inquiry really shines a light on the need for more inclusiv healthcare policies. i think it’s crucial that we involve community groups in the rollout of these new safeguards. also, misspelling aside, the push for real‑time monitoring could be a game‑changer if we get the tech right.
Vinay Upadhyay
May 23, 2024 AT 01:37The depth of the systemic malaise documented in the inquiry warrants a thorough unpacking, so let me lay it out step by step. First, the regulatory capture evident in the blood product approval process created a feedback vacuum where safety signals were muted. Second, the absence of a statutory duty of candour effectively insulated decision‑makers from accountability, allowing misinformation to proliferate unchecked. Third, the compensation framework outlined is hamstrung by ambiguous eligibility criteria, which will inevitably spawn a secondary bureaucracy of claim adjudication. Fourth, the recommended overhaul of clinical training fails to address the cultural inertia that privileges hierarchy over interdisciplinary collaboration. Fifth, the proposed real‑time monitoring systems sound promising, yet their implementation will be riddled with data governance challenges, especially concerning patient privacy. Sixth, the reliance on a single oversight body could re‑centralize power, merely shifting the locus of risk rather than diluting it. Seventh, the recommendation to involve the Public Administration and Constitutional Affairs Committee is a nominal gesture unless it is endowed with enforcement powers and budgetary autonomy. Eighth, the narrative glosses over the intersectional impact on marginalized communities, who historically bear a disproportionate burden in health crises. Ninth, the report’s emphasis on “statutory duty” overlooks the necessity of building a culture of ethical reflexivity within health institutions. Tenth, the suggested public awareness campaigns must be crafted with linguistic inclusivity to avoid alienating non‑native speakers. Eleventh, the technological solutions proposed-like blockchain for traceability-require substantial upfront investment and a skilled workforce that currently doesn’t exist in the NHS. Twelfth, the timeline for these reforms is conspicuously absent, which is a red flag for any policy that aims to be impactful. Thirteenth, the financial logistics of compensating thousands of victims will strain public coffers unless paired with a transparent fiscal plan. Fourteenth, the report’s optimism about “momentum for change” is premature without concrete milestones. Fifteenth, in sum, the inquiry offers a comprehensive checklist, but without binding legislative mandates and cultural transformation, it risks becoming another paper‑thin reform that fades into obscurity.
Eve Alice Malik
May 23, 2024 AT 02:27We need to act now.
Debbie Billingsley
May 23, 2024 AT 03:17The nation's honor demands immediate restitution for those betrayed by our health system. It is unacceptable that bureaucratic inertia continues to deprive victims of rightful compensation. Our government must prioritize these claims above political games, ensuring that justice is not merely a slogan but a living reality for every affected family.
Patrick Van den Berghe
May 23, 2024 AT 04:07While the inquiry is thorough it lacks actionable steps
Josephine Gardiner
May 23, 2024 AT 04:57It is evident that the report’s recommendations require a structured implementation framework with clear timelines, responsible agencies, and measurable outcomes. Without such mechanisms, the proposed reforms risk remaining rhetorical.
Jordan Fields
May 23, 2024 AT 05:47Implementation must be backed by law and enforced consistently.
Divyaa Patel
May 23, 2024 AT 06:37The inquiry’s philosophical musings on trust are profound, yet pragmatic steps are essential. We should blend ethical imperatives with concrete policy tools, ensuring that the future of healthcare is both compassionate and accountable.
Larry Keaton
May 23, 2024 AT 07:27Honestly, the best way forward is to set up a joint task force of doctors, patient advocates, and policymakers to drive the compensation process forward. Let’s stop the bureaucratic delays and get real results.
Liliana Carranza
May 23, 2024 AT 08:17We must channel the outrage into constructive action, rallying both the public and officials to demand swift justice. The future health system depends on our collective voice.
Jeff Byrd
May 23, 2024 AT 09:07Sounds like a plan, but let’s make sure the paperwork doesn’t drown the good intentions. Keep it simple, keep it fast.